National Patient Experience Week Resource Hub
Patient experience week - acknowledge & showcase innovative efforts of clients & highlight strategies to improve patient experience. Get resources here!
Benchmarking board performance: 500 board reviews later
Unlock evidence-based insights into board performance

Prior to the COVID-19 pandemic, telehealth adoption was far from widespread. Despite obvious benefits of improving access, the technology wasn’t in place, consumers weren’t ready, and providers resisted the shift to virtual care.
Then came the pandemic—and the need for social distancing. Suddenly, telehealth was in high demand. With over 80 million telehealth services provided in Australia during 2021.
Insync’s healthcare partner Press Ganey surveyed patients throughout the pandemic regarding their use of and experiences with telehealth, and the results are instructive.
“It’s unlikely that telehealth will retreat to pre-COVID levels now that patients, health systems, hospitals, and medical practices have realised the benefits of virtual care and the right technologies are in place.”
The difference between now and 2019 is that healthcare organisations and providers have invested the time and resources into developing a better system and learning how to use it—and patients have more trust in the technology. It’s time to begin understanding where telehealth works best, where it doesn’t work at all, and how it can most effectively be deployed to meet the needs of patients and of health systems.
To make telehealth visits successful, providers should focus on improving communication skills and interpersonal connections with patients. The following five skills are essential for effective, friction-free telemedicine.
Now that the technology is in place and most people understand how to use it, setting up workflows and processes around telemedicine will finally let health systems, hospitals, providers, and patients take full advantage of telehealth.
By Jessica C. Dudley MD, & Chrissy Daniels, Press Ganey Chief Experience Officer
July/August 2022 – Call for General Practices to participate
In response to high telehealth demands, Insync (an accredited RACGP patient experience survey provider) will be undertaking a national research project to assess and profile the primary care industry’s response to delivering compassionate, connected care to patients through telehealth practices and is seeking your help to support this important initiative.
Participation in this project will allow individual primary care practices to understand and respond in real-time to their patients’ attitudes and perceptions of telehealth and benchmark their performance compared to peer organisations nationally.
REGISTRATIONS ARE NOW CLOSED. ENQUIRE WITHIN.
Contact telehealthstudy@insync.com.au for additional information.
By Jessica C. Dudley MD, & Chrissy Daniels, Press Ganey Chief Experience Officer
Data collected by Press Ganey reveals what’s working in telehealth as well as areas for improvement.
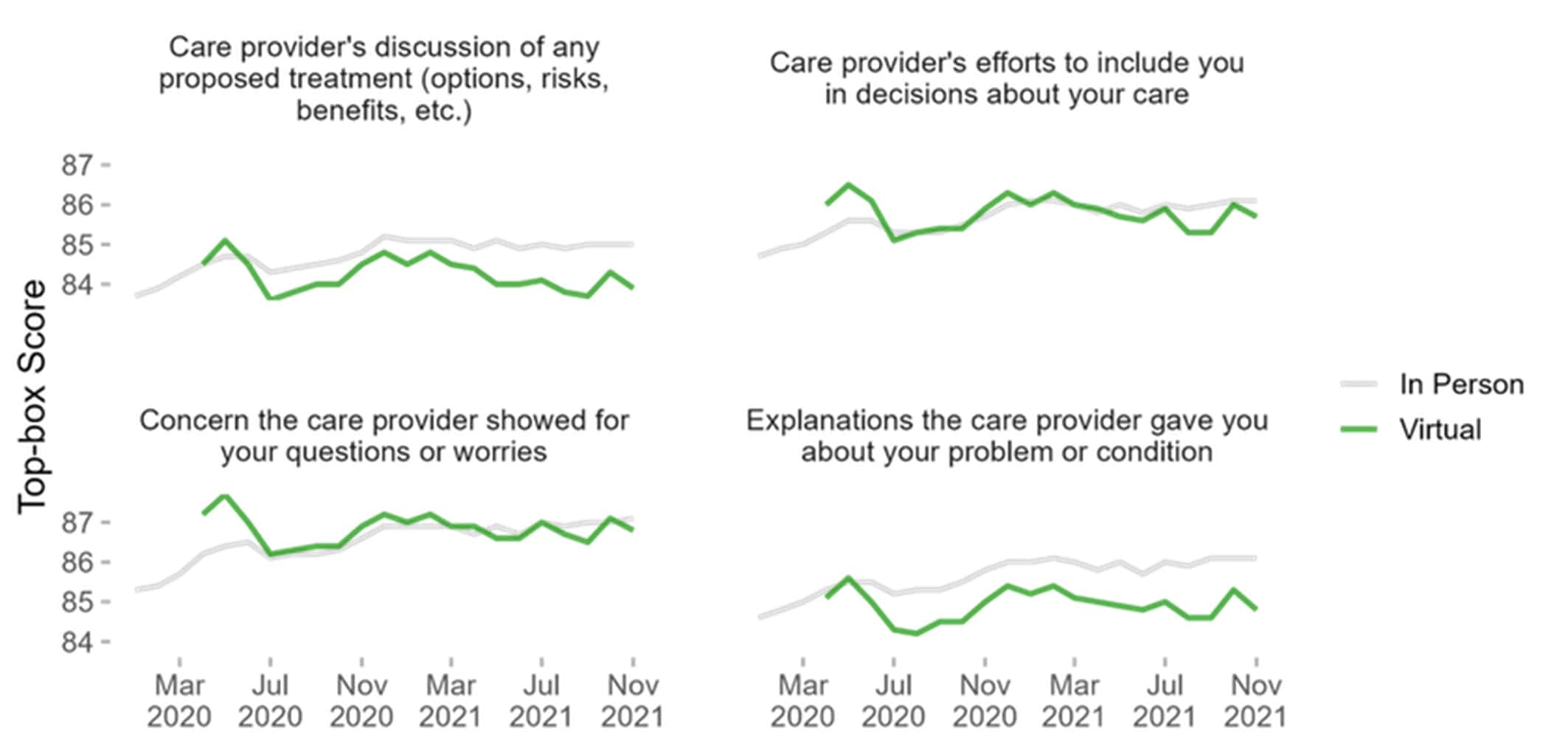
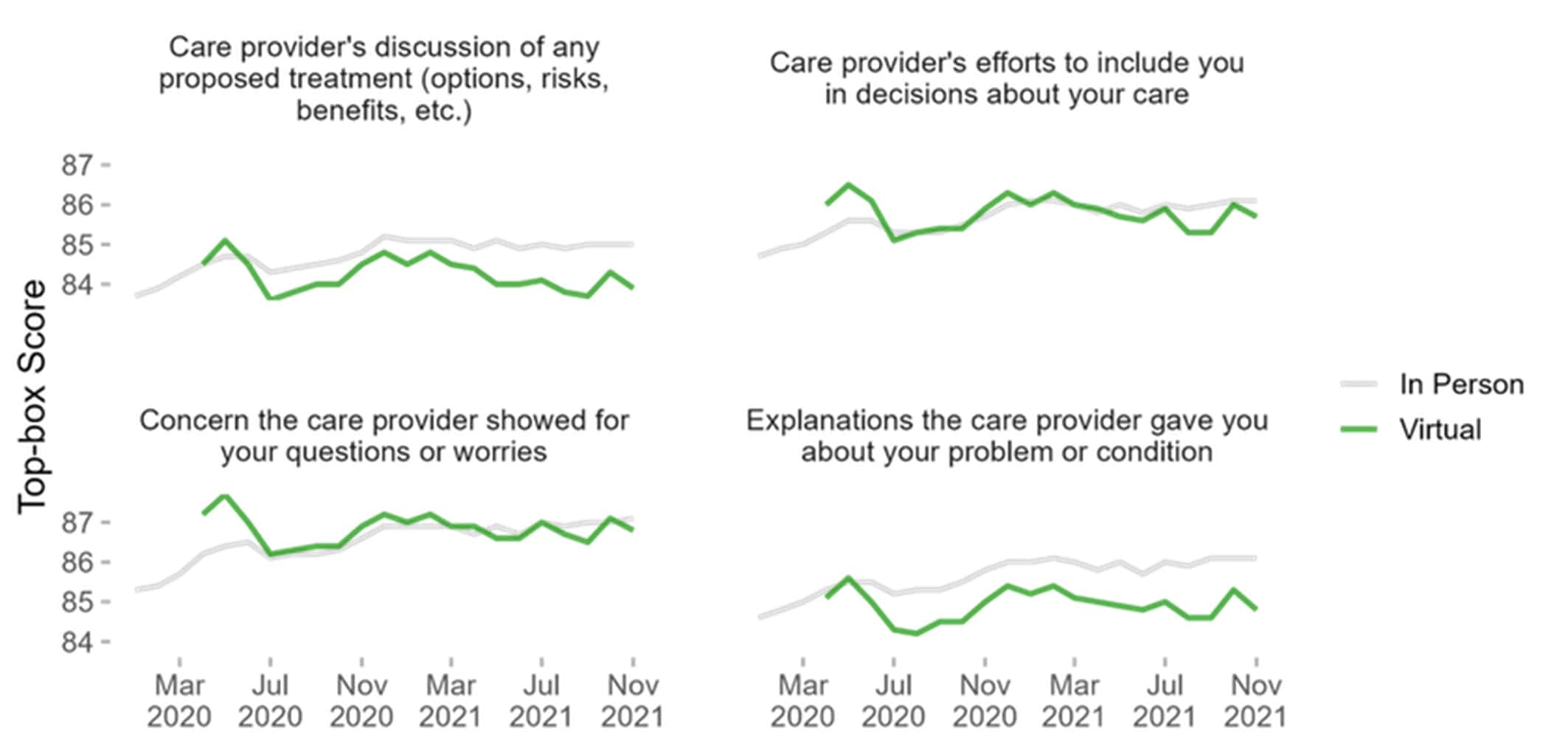
When asked about “providers’ efforts to include you in decisions about your care” and “concern the care providers showed regarding your questions or worries,” patients reported that the virtual and in-person experiences were similar.
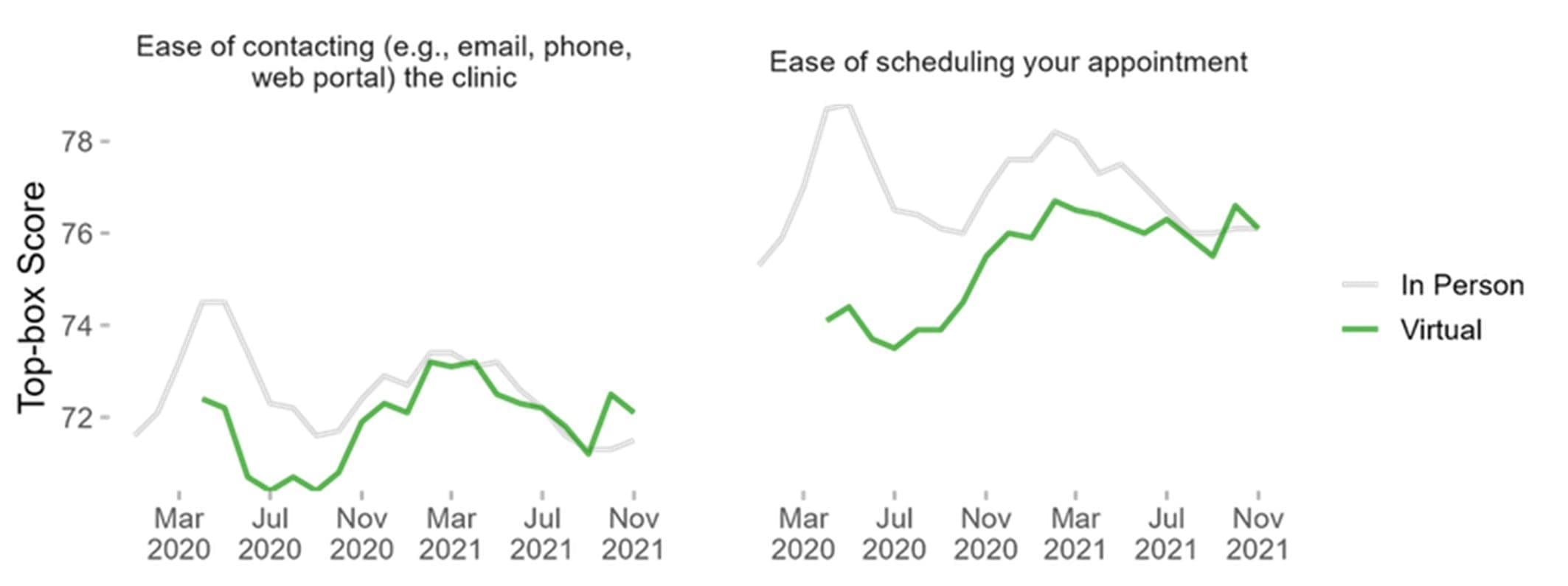
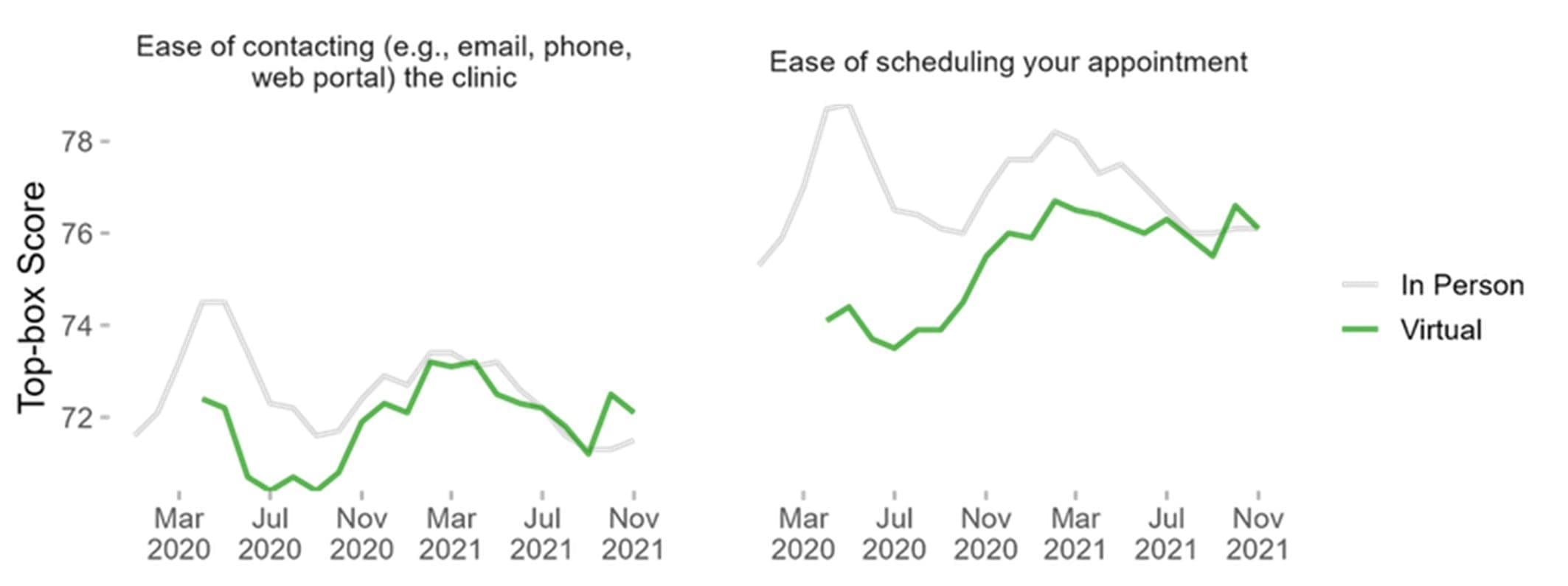
By mid-2021, gaps in the ease of scheduling in-person and virtual appointments had closed, as well as ease of contacting clinics regarding telehealth appointments. This was a shift from early in the pandemic when consumers reported that it was easier to schedule an in-person appointment than a virtual visit.
But virtual care is still in its early stages and providers are still getting up to speed. By November 2021, patients were far less satisfied with providers’ explanations about their problems or conditions during virtual visits than in-person interactions—even though they had started out on par. They were also less satisfied with providers’ discussions of proposed treatment (including options, risks, and benefits) than they had been toward the start of the pandemic.
A new method of care delivery is bound to cause patient experience scores to fluctuate—particularly when telehealth was introduced very quickly, in the throes of a global health crisis. It’s possible that, early on, patients were simply glad they could contact their providers at all, but, as things settled down and they adjusted to the “new normal,” their expectations rose.
Throughout the pandemic, patients’ “Likelihood to Recommend” their provider for virtual vs. in-person care was extremely close. But during this same timeframe, their “Likelihood to Recommend” the practice was much lower for virtual care than in-person visits (though that measure is slowly making up ground). There’s certainly room for improvement in operations for both types of visits—particularly around how well the staff worked together to provide care.
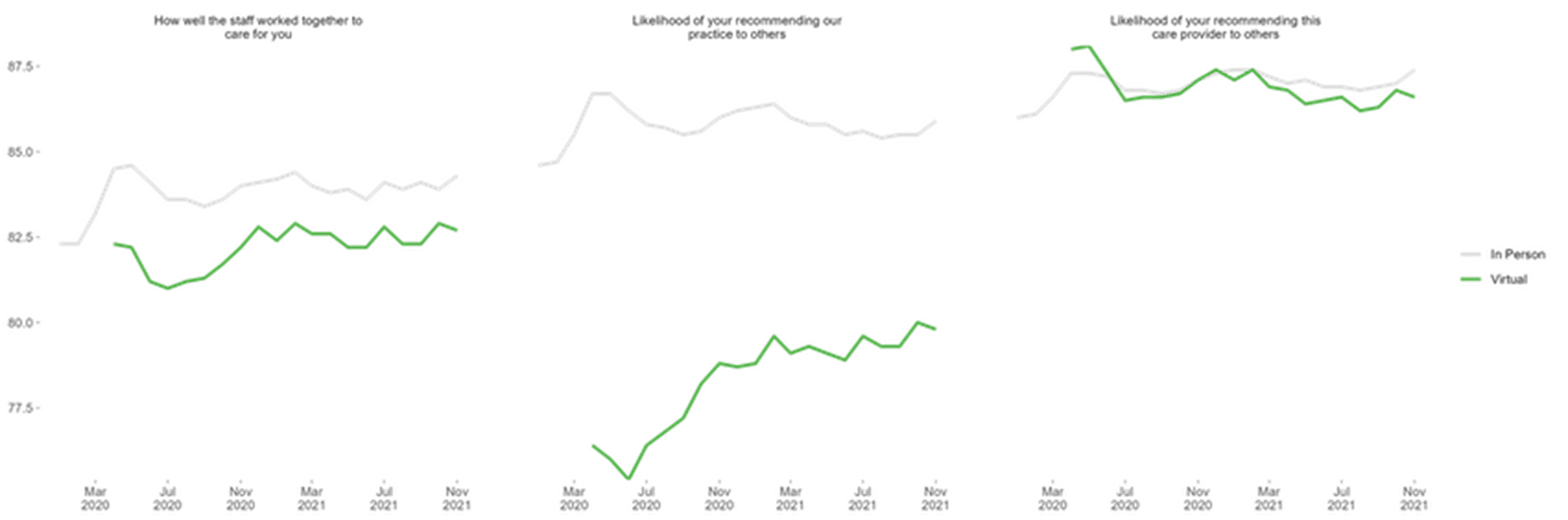
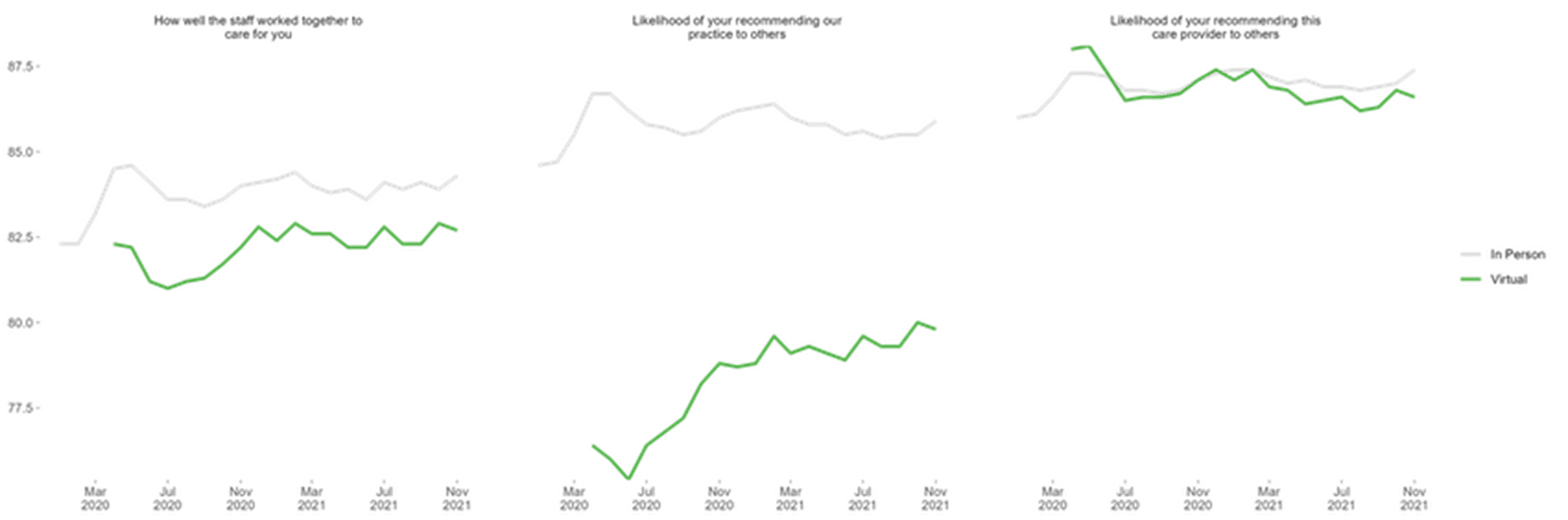
This discrepancy likely stems from the user experience with the technology as well as the expectation setting. At an in-person appointment, patients generally know what to expect from a logistical standpoint: checking in at a desk and sitting in a waiting room until their appointment time.
At a virtual appointment, the process is less clear. A virtual waiting room is sometimes an idle telephone, a blank screen, leaving patients to wonder if they’ve been forgotten, if they used the wrong platform, or if they followed the instructions properly.
Ensuring the logistics of a virtual visit—connecting, checking in, waiting, talking to the provider, etc.—are as straightforward as each step of an in-person visit is critical to making telehealth available across the healthcare system. Training staff and clinicians on how to better communicate virtually must also be prioritised.
Clinicians and staff must work together to develop an advanced team-based care approach for telehealth —one that reflects the in-person experience. During an in-office visit, a practice manager, nurse or medical assistant may meet with the patient first to review medications, update their medical history, discuss symptoms or problems, and check their vitals. This person may take notes and assist with any forms or documentation as the doctors sees them. Then, after the consultation, a nurse may review the next steps with the patient. This approach should also be used in telemedicine, with virtual visits beginning before the doctor enters the “room.”
Patient experience week - acknowledge & showcase innovative efforts of clients & highlight strategies to improve patient experience. Get resources here!
Learn about the latest safety culture trends and how to create a safe workplace environment. Insync Insights help show you how.
Discover the latest trends and insights on employee physician engagement. We provide resources to help employees and physicians to create a better healthcare experience.
Register to participate in Insync's national study assessing the healthcare's response to delivering telehealth practices and gain valuable patient feedback.
We use cookies to enhance your experience. Further use is considered consent. You can read more about cookies in our Privacy Policy.


You’ll always get a real person when you contact Insync.
Let's get started